RGUHS Nat. J. Pub. Heal. Sci Vol No: 17 Issue No: 3 pISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India
2Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India
3Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India
4Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India
5Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India
6Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India
7Dr. Neha Mustare, Post Graduate, Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India.
*Corresponding Author:
Dr. Neha Mustare, Post Graduate, Department of Oral and Maxillofacial Surgery, Al Badar Rural Dental College & Hospital, Kalaburagi, Karnataka, India., Email: nehamustare96@gmail.com
Abstract
Sialoliths, comprising 30% of all salivary gland diseases, can lead to excretory duct obstruction. Predominantly affecting the submaxillary gland (83 to 94%), followed by the parotid (4 to 10%) and sublingual glands (1 to 7%), these concretions have an average size ranging from 6 to 9 mm. We present a case of 34-year-old male presented with an extra-large sialolith in the right parotid duct. The diagnosis was confirmed through clinical examination, panoramic radiography (OPG), and CT scan. The treatment included intra-oral sialolithotomy along with the administration of oral antibiotics and analgesics. Parotid gland calculi, typically unilateral and more prone to affect the duct than the gland itself, are less prevalent than subman-dibular calculi. The choice of treatment for sialoliths depends on factors such as size and location.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Salivary duct lithiasis involves the obstruction of a salivary gland or its duct by calcareous stones, causing the gland to swell and possibly become infected, which can result in chronic sialadenitis.1
There is a tendency for male patients to be more affected, especially when it comes to lithiasis in the parotid gland.1 Typically, this condition manifests in individuals between their 3rd and 6th decades of life. Nonetheless, it does not favour one side over the other, potentially manifesting as multiple and bilateral conditions.2 When considering the location of the sialoliths within the salivary duct system, intraductal sialoliths are more frequently encountered than intraglandular ones.3
Parotid calculi are often unilateral, primarily found within the duct, and their size tends to be less than 1 cm. For sialoliths that do not appear on radiographs, sial-endoscopy may be necessary, as approximately 40% of the parotid and 20% of submandibular stones do not exhibit radiopacity. Despite ongoing research, the exact causes and mechanisms behind the formation of salivary calculi remain not fully understood. Decisions regarding management are influenced by considerations like the size, mobility, and position of the sialolith, in addition to the existence of strictures.4
Case Presentation
A 34-year-old man came to our hospital for assessment of a hard lump in his right cheek. He had been dealing with swelling for two years. He reported the pain as being localized, constant, and sharp, especially inten-sifying when eating. Notably, there was no history of injury to the area. Regarding his dental history, he was previously diagnosed with stage 3 oral submucous fibrosis five years prior, for which he received conservative treatment involving intralesional injections of 1500 IU hyaluronidase (1 ml) combined with triamcinolone acetonide (10 mg/ml), alongside topical antioxidants and active mouth opening exercises. At the time of his visit, his mouth could open to 35 mm. He had no other significant medical history.
During the extraoral examination, there was a notice-able swelling on the right side of the face. This swelling had a diffuse appearance, spreading about 2 cm to the side from the nose's ala towards the front and extending 2 cm forward from the ear towards the back. The swelling measured roughly 3 x 3 cm (Figure 1). The skin covering the swelling was smooth and taut, showing no signs of secondary alterations. Upon palpation, the mass felt hard and was not painful to touch.
Upon intraoral examination, the patient demonstrated a typical mouth opening capacity with no involvement of the teeth. A swelling was noted in the right buccal mucosa, starting from the first molar and extending back to the entrance of the right Stensen's duct. This swelling reached up to 2 cm below the upper buccal sulcus at its highest point and descended to the occlusal plane level at its lowest. The Stensen's duct opening showed signs of slight inflammation and redness. Bi-digital palpation did not express any pus from the duct, yet there was a noticeable decrease in the flow of saliva.
A CT scan was performed, which showed a significant intraductal calcification with dimensions of 2.3 cm by 1.7 x 1.3 cm. This finding corroborated the initial suspicion of a sialolith in the right parotid duct (Figure 2). Due to the stone's closeness to the duct's opening, the choice was made to surgically extract it through an intraoral method (Figure 3).
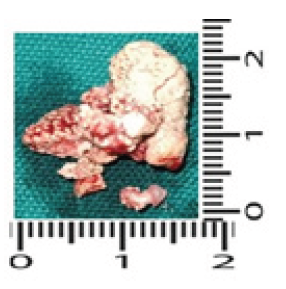
Post-operation, the widened duct was left unsutured. The patient received prescriptions for antibiotics and pain relief medication and was recommended to chew on lemon slices regularly to stimulate salivary flow During subsequent follow-up appointments, there were no reported recurrences of pain or swelling. (Figure 4) presents the dimension of the extracted stone.
Discussion
Sialolithiasis is quite prevalent, making up to 30% of all salivary gland conditions.1 In our recent case study, our patient was a 34-year-old male, which corresponds to the commonly observed age range of this disease (30-60 years). The precise origins and progression of salivary stones are still subjects of active research. Numerous theories have been suggested to elucidate their etiology, including mechanical issues, inflammation, chemical reactions, nerve-related influences, infections, and the introduction of foreign bodies. Classic models propose that sialoliths develop in two stages: (1) the creation of a core from salt precipitation combined with organic materials, and (2) the buildup of additional organic and inorganic layers. Another hypothesis, known as the retrograde theory, suggests that materials or bacteria from the mouth might enter the salivary ducts, providing a starting point for calcification. While hypercalcemia has been linked to sialolithiasis in animal research, this connection remains unproven in humans, leading to the absence of dietary guidelines concerning calcium intake for preventing salivary stones. The exploration of these and other possible causes continues to enhance our understanding and prevention strategies for this condition.9
Symptoms of salivary gland or duct obstruction with a sialolith typically present as swelling of the salivary duct during eating for no apparent reason, lasting less than two hours and occasionally accompanied by a transient sharp pain known as salivary colic. The clinical picture is often different and helps in early diagnosis; however, it is important to note that pain is only one symptom and may not be present in approximately 17% of cases.5 Sialoliths are typically unilateral and generally do not lead to dry mouth (xerostomia). These stones are primarily composed of calcium phosphate, with lesser amounts of carbonates as hydroxyapatite, plus minor traces of magnesium, potassium, and ammonium. The ratio of organic to inorganic material varies between submandibular and parotid calculi, with submandibular calculi being approximately 18% organic and 82% inorganic, while parotid calculi show a more balanced ratio at 51% organic to 49% inorganic.6
Sialoliths are usually small in size, typically measuring between 1 mm and less than 1 cm, with a few exceeding 1.5 cm. The average size ranges from 6 to 9 mm. Sialoliths are considered large when they exceed 15 mm in any dimension and they are termed giant if they reach 35 mm or more. The biggest recorded sialolith found in the submandibular gland was 6 cm long.2 They are typically round or oval in shape, have a porous texture, and appear pale yellow. Although parotid stones are typically smaller and less visible on X-rays than submandibular stones, we came across an unusual case where the stone measured 2.3 x 1.7 x 1.3 cm, with a pale yellow colour, a porous texture, and high radiopacity. Ductal stones tend to be elongated, unlike the more oval-shaped stones in the hilar area.2
Besides sialography, other diagnostic methods like CT scans and MRIs provide benefits of low invasiveness and high precision. Sialoendoscopy is an effective technique for viewing intraductal narrowing and signs of inflammation.7
Treatment for sialoliths is chosen based on their size and position. For differential diagnosis, one must consider alternatives like sialadenitis, lymphadenitis, preauricular or sebaceous cysts, benign lymphoid hyperplasia or extra-parotid tumors for superficial masses in the salivary glands. For diffuse swelling not originating from the parotid glands, conditions such as masseter hypertrophy or temporomandibular joint issues should be evaluated. It's also crucial to differen-tiate sialoliths from other soft tissue calcifications since parotid stones often cause pain and swelling, in contrast to asymptomatic calcified lymph nodes or other calcifications.
The approach to treating salivary stones depends on which gland is involved and where the stone is located. For smaller stones, non-surgical methods are usually favored. Individuals with small stones might be advised to utilize natural sialogogues like lemon slices or take sialogogue medications. Medications like pilocarpine, along with short-wave infrared heating, can promote ductal muscle contractions; however, there's a risk of salivary colic with medium to large stones, and these treatments might not fully remove the stone. In cases where conservative treatment does not bring results for parotid stones, sonographically guided extracorporeal shock wave lithotripsy is a viable option. This approach does not require anesthesia, sedation, or analgesia and has been shown to be effective, with up to 50-60% of patients getting rid of stones and 80-90% experiencing relief of symptoms. Nonetheless, one must be aware of the possible risks of causing damage to the gland tissue and resulting in fibrosis with this approach.9
Some researchers support treating sialolithiasis with intraductal penicillin or saline injections, arguing that this method is superior to systemic drug administration due to reduced recurrence and other benefits. For patients with large, proximally located sialoliths, extracorporeal shock wave lithotripsy (ESWL) might be suggested. The use of endoscopic intracorporeal shock wave lithotripsy (EISWL) is growing in stone treatment due to its minimal impact on nearby tissues. Sial-endoscopy, being non-invasive, is advised for managing large stones and cases of ductal obstruction. Limitations of sial-endoscopy are that it may not be offered in all hospitals, cost factors, and limited effectiveness in the treatment of large or complex sialolith.
Complications may include duct wall perforation, lingual and facial nerve paresis, papillary stenosis, and duct stenosis.12 Use of the CO2 laser results in minimal bleeding and scarring. Other benefits include clear vision and fewer post-operative complications, contributing to the growing popularity of CO2 laser treatment.2 One should be aware that surgical interventions might pose a risk to the facial nerve.
Intraoral surgery is generally preferred over extraoral methods because it prevents noticeable scars.8 Parotidectomy should only be contemplated as a final measure, particularly for individuals with multiple infected stones (over 3 mm) in one gland, frequent sialadenitis recurrences, and when less invasive methods and shock-wave lithotripsy have proven unsuccessful.10,11 The least invasive method entails microsurgery to reconnect Stensen's duct. Treatment selection is guided by considerations like the sialolith's size, position, and composition.
Parotid sialolithiasis is less common than submandi-bular sialolithiasis, usually appearing on one side and primarily involving the salivary duct rather than the gland itself. The use of sial-endoscopy has grown as a contemporary method for both diagnosis and treatment. Treatment options are selected based on the size and position of the sialolith.
Conflicts of Interest
Nil
Supporting File
References
1. Srinivas Gadipelly, Srilatha T, et al. Parotid sialolith- a case report and review of literature. International Journal of Contemporary Medical Research 2016;3(4);1211-1213.
2. Ashindoitiang JA, Nwagbara VIC, Ugbem T, et al. Huge sialolith of the submandibular gland: a case report and review of literature. J Int Med Res. 2023;51(1):3000605221148443.
3. Ali Iqbal, Anup Gupta K, Subodh Natu S, et al. Unusually large sialolith of Wharton’s duct. Ann Maxillofac Surg 2012;2(1):70-3.
4. Hills AJ, Holden AM, McGurk M. Sialendoscopy-assisted transfacial removal of parotid calculi. Acta Otorhinolaryngol Ital 2017;37(2):128-131.
5. Giacomo Oteri, Rosa Maria Procopio and Marco Ciccciù. Giant Salivary Gland Calculi (GSGC): Report of Two Cases. Open Dent J 2011;5:90-5.
6. Bodner L. Parotid sialolithiasis. J Laryngol Otol 1999;113(3):266-7.
7. Rust TA, Messerly CD. Oddities of salivary calculi. Oral Surg, Oral Med, Oral Pathol 1969;28 (6):862-865.
8. Torres-Lagares D, Barranco-Piedra S, Serrera- Figallo MA, et al. Parotid sialo-lithiasis in Stensen’s duct, Med Oral Patol Oral Cir Bucal 2006;1;11(1):E80-4.
9. Konstant inidis I, Paschaloudi S, Triaridis S, et al. Bilateral multiple sialolithiasis of the parotid gland in a patient with Sjögren’s syndrome. Acta Otorhinolaryngol Ital 2007;27(1):41-4.
10. Zenk J, Werner G, Hosemann MD, et al. Diameters of the main excretory ducts of the adult human submandibular and parotid gland - a histological study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85(5):576-80.
11. Iro H, Schneider H Th, Fodra C et al. Shockwave lithotripsy of salivary duct stones. Lancet 1992; 30;339(8805):1333-6.
12. Singh PP, Gupta V. Sialendoscopy: introduction, indications and technique. Indian J Otolaryngol Head Neck Surg 2014;66(1):74-8.