RGUHS Nat. J. Pub. Heal. Sci Vol No: 17 Issue No: 4 pISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Kiran R Halkai, Department of Conservative Dentistry & Endodontics, Al Badar Rural Dental College & Hospital, Kalaburgi, Karnataka, India.
2Department of Conservative Dentistry & Endodontics, Al Badar Rural Dental College & Hospital, Kalaburgi, Karnataka, India
3Department of Conservative Dentistry & Endodontics, Al Badar Rural Dental College & Hospital, Kalaburgi, Karnataka, India
*Corresponding Author:
Dr. Kiran R Halkai, Department of Conservative Dentistry & Endodontics, Al Badar Rural Dental College & Hospital, Kalaburgi, Karnataka, India., Email: drkiranhalkai@gmail.com
Abstract
Background: Self-adhesive composite resins are a newer class of restorative materials that combine the properties of self-etching bonding systems and composite resin into a single system. Addition of chitosan nanoparticles (Csnps) into composite resins has been shown to enhance antimicrobial activity and improve physical properties. However, the effect of adding Csnps to self-adhesive composites has not been adequately investigated.
Aim: To compare the microleakage of Class V cavities restored with self-adhesive resins and conventional flowable composites, both with and without 0.2% Csnps.
Method: Sixty human extracted single-rooted mandibular premolars were cleaned, and Class V cavities of standard dimensions were prepared on the facial surfaces. The specimens were randomly divided into five groups (n=12) for restoration: Group 1- Self-adhesive composite (SAC); Groups 2- SAC with 0.2% Csnps; Group 3- Flowable composite; Group 4- Flowable composite with 0.2% Csnps; and Group 5- No restoration (control). All specimens were immersed in methylene blue dye for 24 hours, washed with sterile water, sectioned buccolingually, and evaluated for microleakage in the occluso-gingival direction under a stereomicroscope (16x). Statistical analysis was performed using the Kruskal-Wallis and Mann-Whitney U test (P ≤0.05).
Results: The highest microleakage was observed in Group 5 (control). Flowable composite resin performed better than self-adhesive composite resin, both with and without csnps. Significant differences were found between all groups, except between Groups 1 and 3, and Group 2 with Groups 3 and 4 (P ≤0.05).
Conclusion: Incorporation of Csnps into self-adhesive and flowable composite resins reduced microleakage. Although flowable composite resin showed superior performance compared to self-adhesive resin, the addition of Csnps to self-adhesive composites offers the advantage of a simplified restorative technique while minimizing microleakage in Class V cavities.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Composite resins are the universal choice for most restorations due to their aesthetic appearance and improved properties.1 The major drawback of composites is polymerization shrinkage, which leads to the formation of gaps at the tooth-restoration interface, resulting in microleakage that can cause post-operative hypersensitivity, secondary caries, pulpal pathology, and restoration failure.2
Placing restorative materials with an adequate seal in the cervical area has long been recognized as a challenging and technically demanding task. The main reasons for this include difficulties in isolating the area, accurately inserting the restorative material, shaping it properly, and achieving a smooth finish. As a result, secondary cavities often develop. Furthermore, the cervical region presents challenges due to the constant masticatory load exerted on the teeth, which leads to deformation. To mitigate these concerns, it is essential to select a material with a high degree of flexibility and low rigidity. This characteristic allows the restoration to exhibit greater adaptability and resilience, enabling it to harmoniously accommodate the natural movements of tooth during occlusal forces. Given these challenges, there is a continuous quest for a suitable restorative material that exhibits excellent adhesive properties, minimizing the microleakage, particularly for Class V lesions.3
Composite materials have been widely recognized as the preferred choice for restoring Class V lesions.4 Their low modulus of elasticity allows for better adaptation and flexion with the natural tooth, minimizing the risk of debonding under load, in comparison to other materials. Composite materials offer enhanced mechanical properties and improved wear resistance. Moreover, flowable composites have demonstrated superior performance in Class V restorations. Their reduced polymerization shrinkage forces contribute to a decreased likelihood of microleakage.5
Recently, a new class of composite resins, called compobonds or self-adhesive resins, have been introduced. These materials combine the properties of self-etching bonding systems and composite nanofillers into a single system. They do not require a separate step for the application of etchant or bonding agent. Therefore, they bring tangible benefits, such as shortening the treatment time and simplifying the procedure.6,7 Constic (DMG, Hamburg, Germany) is a self-adhesive flowable composite resin containing methacrloxydecyl-dihydrogen-phosphate-(MDP), ethoxylated bisphenol A dimethacrylate (EBADMA), bisphenol A-glycidyl methacrylate, triethylene glycol dimethacrylate (TEGDMA), urethane dimethacrylate (UDMA), 2-hydroxy ethyl methacrylate (HEMA), and 1,6-hexanediol dimethacrylate (HDMA) monomers. MDP holds longer and more hydrophobic spacer chains and forms stable MDP-calcium salts, thus minimizing decalcification and creating strong chemical bonds with hydroxyapatite. It is suitable for small Class I, II and V cavities, offering superior aesthetics and reduced clinical application time, since no separate etching or bonding system is needed. In addition, it demonstrates improved clinical performance.8,9
Chitosan is an emerging natural antimicrobial agent which is partially or completely deacetylated derivative of chitin, a biomaterial extracted from seafood shells. It has favourable properties such as low toxicity, high biodegradability, and biocompatibility.10 Different concentrations of chitosan nanoparticles (Csnps) have been incorporated in restorative materials such as GIC, dentin bonding agents and composite resins for enhancing their properties like antimicrobial efficacy, shear bond, and pushout bond strength.11
The literature is scare regarding the incorporation of Csnps into self-adhesive resins with respect to the evaluation of microleakage. Therefore, the goal of this study was to assess microleakage in Class V cavities using a self-adhesive flowable composite and a conventional flowable nanocomposite resin, both with and without Csnps.
Materials and Methods
Ethical clearance was obtained from the institutional ethics committee (reference no: ICE/2020-21/24), and all the procedures were performed in accordance with the approved protocol.
Sixty human single-rooted mandibular premolars extracted for orthodontic or periodontal purposes were collected. Ultrasonic scaler (Guilin Woodpecker, Medical Instrument Co. Ltd, Guilin, China) was used to remove any debris or tissue remnants, following which the teeth were stored in 0.5% sodium hypochlorite (NaOCl) solution for 15 minutes, rinsed with water, and stored in normal saline until further use.
Preparation of the specimens
To ensure consistent dimensions, Class V cavities measuring 2 mm in width, 2 mm in depth, and 2.5 mm in length were marked with a black marker and prepared on the facial surface of each specimen using a straight fissure bur (Mani, Tochigi, Japan) in a high-speed handpiece (NSK, Pana Air, Japan). The gingival margins were placed 1 mm above the CEJ. The measurement of the cavities was verified using a graduated periodontal probe (GDC Fine Crafted Dental Pvt. Ltd., Hoshiarpur, India) and a divider. Subsequently, the prepared surfaces underwent irrigation with distilled water and were air dried. The specimens were then arbitrarily segregated into six groups (n=12) and restored as follows:
Group 1- Self-adhesive flowable (SAF) composite
Group 2- SAF with 0.2% Csnps
Group 3- Flowable nanocomposite (FNC)
Group 4- FNC with 0.2% Csnps
Group 5- No restoration (Control group)
In Group 1, the self-adhesive flowable composite resin, Constic (DMG, Hamburg, Germany), was placed according to the manufacturer’s instructions in 1-mm increments using a carrier and condensed properly. In Groups 3 and 4, the self-adhesive universal bonding agent Tetric N-Bond (Ivoclar Vivadent, Schaan, Liechtenstein, Germany) was applied, and light cured with a curing unit (VIP, Bisco Inc., Schaumburg, IL, USA) for 20 seconds, followed by placement of the flowable composite resin Tetric N-Flow (Ivoclar Vivadent, Schaan, Liechtenstein, Germany) in 1-mm increments until the cavity was completely filled. In Groups 2 and 4, the composite resins were mixed with commercially available 0.2% Csnps powder particles (NRL, Ahmedabad, India) in a 3:1 ratio, following Mirani et al. 12 The materials were blended in a glass beaker in a dark room using a glass rod until a homogenous mix was obtained, then placed into the cavities in 1-mm increments and light cured for 20 seconds. In Group 5 (control), no restoration was performed; the prepared cavities were coated with two layers of nail varnish. In all experimental groups, restorations were finished and polished using a composite polishing kit (Shofu, Kyoto, Japan). All specimens were preserved in distilled water (Water Care Technologies, Nagpur, India) for 24 hours prior to testing.
Evaluation of microleakage
To evaluate the penetration of dye, all the specimens were coated with a double layer of nail varnish, leaving a 1 mm margin between the tooth and the restoration. To prevent leakage, the apices of the roots were sealed using sticky wax (JD Wax and Manufacture, Rajkot, India). The specimens were then immersed in methylene blue dye (Nice Chemicals Pvt Ltd, India) at 37˚C for 24 hours, rinsed with distilled water, and the varnish coatings were scrapped off. The samples were subsequently washed and air dried. The root portion of each tooth was cut horizontally 4 mm below the CEJ using a low-speed diamond disk (Mani, Tochigi, Japan), and the coronal portion was sectioned buccolingually through the midpoint of the restoration. Microleakage in the occluso-gingival direction was evaluated on both halves using a stereomicroscope (Labsol Enterprise, Haryana, India) at 16x magnification. For each specimen, the section showing the highest microleakage was recorded. The extent of dye penetration was assessed according to the scale described by Varshneya et al.13
- No dye penetration
- Penetration up to 1/3rd of cavity depth
- Penetration up to 1/3rd - 2/3rd cavity depth
- Penetration more than 2/3rd cavity depth, but not involving axial wall
- Penetration involving axial wall
Statistical analysis
The data collected were summarized using descriptive statistics as mean and standard deviations and statistically analysed with the Statistical Package for Social Sciences (SPSS) software version 22 (IBM Statistics, Chicago, USA). The Kruskal-Wallis test and Mann-Whitney U test were applied, with the level of significance set at P ≤0.05.
Results
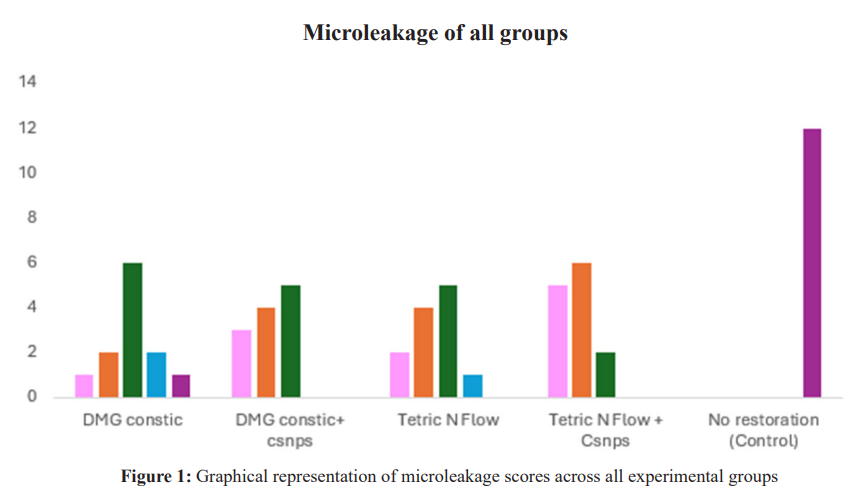
The Kruskal-Wallis test revealed the highest microleakage in Group 5 (control), followed by Groups 1, 3, and 2, while the least microleakage was noted in Group 4.The differences among the groups were statistically significant (Table 1 and Figure 1). The Mann-Whitney U test showed significant differences between all groups, except between Groups. 1 and 3, Groups 2 and 3, and Groups 2 and 4 (P ≤0.05) (Table 2).
Discussion
The effectiveness of a restorative material used depends on its ability to establish strong adhesion to the tooth and create an impermeable seal at the restorative margins, which is crucial for preventing the ingress of fluids and microorganisms that lead to microleakage and secondary caries. The gold standard for microleakage is achieved by the use of dye penetration technique in vitro compared to in vivo conditions of oral cavity, since the salivary proteins tend to seal the margin of resin-restoration interface. The dye leakage model is comparatively easier to perform and simple than the bacterial model.14 Hence this model was used in the present study.
To improve the physical properties of composite the incorporation of Csnps.15 Chitosan has shown potential in preventing the occurrence of recurrent caries. However, it is crucial to ensure that the addition of Csnps does not compromise the adhesive properties of the material or increase the risk of microleakage at the restoration margins. Therefore, researchers aimed to strike a balance between improving material properties and maintaining the integrity of the restoration interface, ultimately leading to successful and long-lasting restorations.
In the present study, both composite resins used were flowable composites placed in low-thickness increments. Hernandes et al., found that restorations with low thickness of flowable composite showed reduced microleakage, indicating that controlling thickness of the composite has a significant impact on minimizing microleakage.16
In this study, 0.2% Csnps were incorporated into composites, as Mohamed et al., reported the highest bond strength values with 0.2% Csnp-containing composites, while the lowest values were observed at 2.5%. Similarly, Satheesh et al., noted that chitosan concentrations of 2.5 wt% and below allow uniform distribution within composite resins without compromising their physical properties. Moreover, Szczepanska et al., found that using low concentrations of chitosan (up to 0.5%) provides protection to pulp cells.17,18,19
In the present study, incorporating 0.2% Csnps into self-adhesive and conventional flowable composites resulted in better resistance to microleakage compared to without Csnps. The study results are in line with Thomas et al., who reported that chitosan pretreatment of Class II cavities before placing universal adhesives and composite resins resulted in microleakage reduction.20 In another study by Deb et al.,the microleakage of Class V cavities was found to be less in chitosan-incorporated nanohybrid composite resin and no significant difference was found with usage of either total etch or self-etch adhesives.21 Satheesh et al., stated that composite resin benefits from incorporation of chitosan, as it acts as a filler and occupies voids within the resin through its reactive amine and hydroxyl groups.18 In addition, its high nitrogen content (approximately 6.89%) and NH2 chains enhance adhesion between the components of the composite resin, thereby preventing the leakage of monomers and hydrolytic bond degradation, ultimately reducing volumetric shrinkage and microleakage. Similarly, Elaska et al., stated that the binding properties of the adhesive system are not affected by 0.12% and 0.25% (w/w) chitosan, as the amine groups in chitosan enhance stability by potentially increasing cross-linking with the resin, further improving the thermal stability.22 This mechanism may have contributed to the reduction in microleakage observed in this study with the addition of Csnps to both composites.
The present study findings showed higher microleakage in the self-adhesive composite resin compared to the conventional nanofilled composite resin; however, the difference was not statistically significant. This is in accordance with Hosseinipour et al., who reported that conventional fissure sealants with total-etch or self-etch adhesives demonstrated lower microleakage compared to self-adhesive composites.23 Similarly, Rangappa et al., reported improved adhesion with the flowable resin composite Tetric N-Flow compared to the self-adhesive composites Constic and Dyad Flow. Self-adhesive composites function in a manner similar to self-etch adhesives.24 The microleakage observed in self-adhesive materials may be attributed to inadequate micromechanical retention between the restorative material and tooth structure, resulting from their limited etching capacity. In contrast, conventional etching increases the enamel surface area and creates micro-retentive tags, thereby enhancing bonding. Self-etch materials, however, do not etch enamel as deeply as phosphoric acid, which may compromise enamel bonding. Etching with phosphoric acid followed by rinsing exposes the underlying prismatic structure, facilitating better resin cement bond. However, this effect is not seen with self-etch materials.20 This could explain the higher microleakage observed in the self-adhesive composite groups in the present study. Conversely, Vichi et al., reported that self-adhesive composites exhibit higher hygroscopic expansion due to increased water sorption by acidic resins, which reduces polymerization shrinkage and improves marginal sealing. Similarly, Chalas et al., found that self-adhesive composites performed better clinically with adequate adhesion. In contrast, Maj et al. reported poor marginal adaptation and greater surface roughness for the self-adhesive composite Vertise Flow.7,9,25
As no studies are currently available comparing the self-adhesive composite resin Constic with other composite resins containing Csnps, the findings of the present study, along with existing literature, suggest that the incorporation of Csnps reduces microleakage in both types of composite resins evaluated. Notably, incorporating Csnps into self-adhesive composites offers additional advantages, including simple and fast placement, elimination of separate etching and bonding steps, and the potential for more stable bonding, which enhances adhesion between the composite and tooth structure while reducing microleakage. However, certain limitations of this study must be acknowledged, including the relatively small sample size, the methods employed, the type of composites and adhesives tested, and the concentration of Csnps used, all of which may have influenced the results. Therefore, further in vitro and in vivo investigations are needed to evaluate the material's long-term durability, adhesive capacity, aesthetic outcomes of Csnp-modified composites. Such investigations will provide a deeper understanding of the material's performance and its potential clinical applicability.
Conclusion
Microleakage was lower in the conventional flowable nanocomposite compared with the self-adhesive composite resin, both with and without Csnps. However, the addition of Csnps to self-adhesive composites simplifies the restoration procedure and may enhance longevity by minimizing the microleakage in Class V cavities.
Conflict of interest
None
Supporting File
References
- Perdigão J, Lambrechts P, Van Meerbeek B, et al. The interaction of adhesive systems with human dentin. Am J Dent 1996;9:167-73.
- Goracci G, Mon G, Bazucchi M. Marginal seal and biocompatibility of a fourthgeneration bonding agent. Dent Mat 1995;11:343-347.
- dos Reis Perez C, Gonzalez MR, Prado NA, et al. Restoration of non-carious cervical lesions: when, why, and how. Int J Dent 2012;2012:687058.
- Srirekha A, Bashetty K. A comparative analysis of restorative materials used in abfraction lesions in tooth with and without occlusal restoration: three-dimensional finite element analysis. J Conserv Dent 2013;16:157-161.
- Pereira R, Giorgi MC, Lins RB, et al. Physical and photoelastic properties of bulk-fill and conventional composites. Clin Cosmet Investig Dent 2018;10:287-296.
- Poitevin A, De Munck J, Van Ende A, et al. Bonding effectiveness of self-adhesive composites to dentin and enamel. Dent Mater 2013;29:221-230.
- Vichi A, Goracci C, Ferrari M. Clinical study of the self-adhering flowable composite resin Vertise Flow in Class I restorations: Six-month follow-up. Int Dent 2011;5:14-24.
- Wang R, Shi Y, Li T, et al. Adhesive interfacial characteristics and the related bonding performance of four self-etching adhesives with different functional monomers applied to dentin. J Dent 2017;62:72-80.
- Chałas R, Kami´nska-Pikiewicz K, ZubrzyckaWróbel J, et al. Compobond-composite or bond? Proprietary clinical observation of Vertise Flow material. Dent Forum 2015;42:11-15.
- Limapornvanich A, Jitpukdeehodintra S, Hengtrakool C, et al. Bovine serum albumin release from novel chitosan-fluoroaluminosilicate glass ionomer cement: Stability and cytotoxicity studies. J Dent 2009;37:686-690.
- Diolosà M, Donati I, Turco G, et al. Use of methacrylate-modified chitosan to increase the durability of dentine bonding systems. Biomacromolecules 2014;8:4606-13.
- Mirani SA, Sangi L, Kumar N, et al. Investigating the antibacterial effect of chitosan in dental resin composites: A pilot study. Pakistan Oral Dent J 2015;35:304-306.
- Varshneya K, Benjamin S, Naveen DN, et al. Microleakage in class V cavities restored with composite resin using chitosan and consepsis as the cavity disinfectants. Adv Tissue Eng Regen Med 2017;2:176-180.
- Jacobs MS, Windeler AS. An investigation of dental luting cement solubility as a function of the marginal gap. J Prosthet Dent 1991;65:436-42.
- Abraham D, Thomas AM, Chopra S, et al. A comparative evaluation of microleakage of glass ionomer cement and chitosan- modified glass ionomer cement: an in vitro study. Int J Clin Pediatr Dent 2014;7:6-10.
- Hernandes NM, Catelan A, Soares GP, et al. Influence of flowable composite and restorative technique on microleakage of class II restorations. J Investig Clin Dent 2014;5:283-8.
- Mohamed AM, Nabih SM, Wakwak MA. Effect of chitosan nanoparticles on microtensile bond strength of resin composite to dentin: An in vitro study. Braz Dent 2020;23:1-10.
- Satheesh B, Tshai KY, Warrior NA. Effect of chitosan loading on the morphological, thermal, and mechanical properties of diglycidyl ether of bisphenol A/hexamethylenediamine epoxy system. J Compos 2014;31:273-79.
- Szczepanska J, Pawlowska E, Synowiec E, et al. Protective effect of chitosan oligosaccharide lactate against DNA double-strand breaks induced by a model methacrylate dental adhesive. Med Sci Monit 2011;17:201-8.
- Thomas AA, Shenoy N, Kini S, et al. Comparative evaluation of the microleakage of two bonding systems pretreated with chitosan nanoparticles and restored with composite resin: An in vitro study. Engineering Proceedings 2023;59:110.
- Deb A, Pai V, Akhtar A, et al. Evaluation of microleakage of micro hybrid composite resins versus chitosan-incorporated composite resins when restored in class V cavities using total etch and self-etch adhesives: An in vitro study. Contemp Clin Dent 2021;12:346-351.
- Elsaka SE. Antibacterial activity and adhesive properties of a chitosan-containing dental adhesive. Quintessence Int 2012;43:603-13.
- Hosseinipour ZS, Heidari A, Shahrabi M, et al. Microleakage of a self-adhesive flowable composite, a self-adhesive fissure sealant and a conventional fissure sealant in permanent teeth with/without saliva contamination. Front Dent 2019;16:239-247.
- Rangappa A, Srinivasulu J, Rangaswamy V, et al. Comparative evaluation of bond strength of self-adhering flowable composites to the dentin prepared with different burs: An in vitro study. J Conserv Dent 2018;21:618-621.
- Maj A, Trzcionka A, Twardawa H, et al. A comparative clinical study of the self-adhering flowable composite resin vertise flow and the traditional flowable composite resin premise flowable. Coatings 2020;10:800.