RGUHS Nat. J. Pub. Heal. Sci Vol No: 17 Issue No: 4 pISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Private Practice, Namah Dental Clinic,Vadodara, Gujarat, India
2Dr. Harshit Naik, Namah Dental Clinic, Vadodara, Gujarat, India.
*Corresponding Author:
Dr. Harshit Naik, Namah Dental Clinic, Vadodara, Gujarat, India., Email: drharshitnaik@gmail.com
Abstract
The maxillary first molar is renowned for its anatomical complexity, particularly the presence of multiple canals, including the elusive MB2 canal. Inability to identify and adequately treat this canal can result in treatment failure and subsequent complications. Therefore, clinicians must possess a thorough understanding of anatomical variations and employ advanced techniques to improve success rates. This case report highlights the successful identification and negotiation of the MB2 canal in a maxillary first molar, a challenging yet crucial aspect of endodontic treatment. A 25-year-old male presented with asymptomatic irreversible pulpitis in the maxillary right first molar. Clinical examination revealed deep caries without tenderness on percussion or palpation, while radiographic examination showed extensive decay and periapical radiolucency. The MB2 canal was located and negotiated using a combination of hand files and rotary instruments under copious irrigation. Patency was confirmed, and the canal was thoroughly debrided and shaped to facilitate obturation. Root canal filling was then completed with gutta-percha and sealer. This report underscores the significance of MB2 canal exploration in maxillary first molars and emphasizes the role of contemporary endodontic techniques in managing complex anatomical variations.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
More often than not, we encounter additional roots, extra canals, complicated root canal anatomy during routine root canal procedures. The true success of an endodontist lies in identifying these anomalies and manage them effectively. Some are visible to the naked eyes, some can be seen with magnification aids, some at the very beginning of the procedure and others only as the procedure progresses. Each root canal is unique and requires both keen observation and open mind to negotiate, clean and obturate. This is the foundation of successful endodontic treatment.
Although advanced aids offer a clear advantage in such cases, careful attention to visible anatomical variations can be equally valuable. Routine IOPAs and proper visualisation of the dentinal floor often provide important clues about existing variations in a particular tooth.
Case Presentation
A 25-year-old male patient reported to the clinic with the chief complaint of decay in the upper back tooth region. He did not experience pain but reported difficulty in chewing food for the past one year. His medical history was non-contributory, and there was no history of pain or swelling associated with the affected tooth.
On physical examination, the maxillary right first molar (16) had a deep carious lesion. Palpation of the buccal and palatal aspects revealed no tenderness. The tooth was non-tender on vertical percussion, showed no mobility, and periodontal probing depths were within physiologic limits.
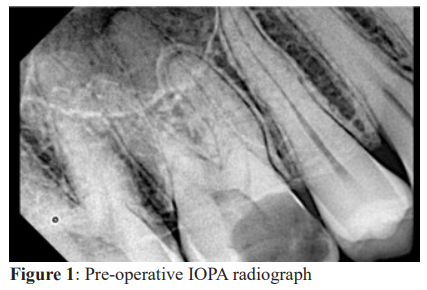
A preoperative IOPA radiograph revealed a deep carious lesion involving the pulp of tooth 16, with periodontal ligament widening in the mesiobuccal root and a periapical lesion associated with the palatal root (Figure 1).
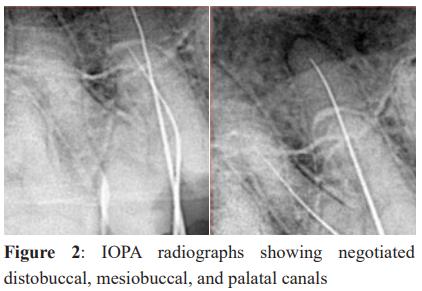
Based on these findings, a diagnosis of asymptomatic irreversible pulpitis irt 16 was established. The proposed treatment plan was non-surgical endodontic therapy, which the patient accepted. Local anaesthesia was administered using 2% lignocaine with 1:80000 adrenaline. An access cavity was prepared, and initial exploration was performed with size 8 K-files. Three canals – mesiobuccal, distobuccal, and palatal, were identified and negotiated (Figure 2).
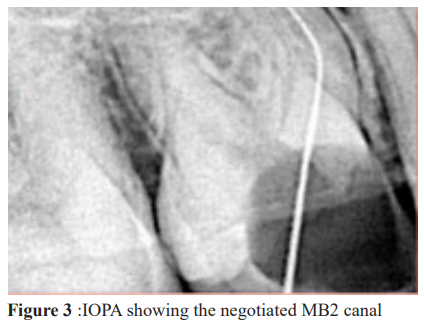
Following the dentinal map, the presence of an additional canal was suspected, although it could not be negotiated. Hence, shaping and cleaning of the three previously negotiated canals were completed. After biomechanical preparation with 17% EDTA and copious irrigation using normal saline and 5.25% NaOCl, the orifice of the suspected canal near the mesiobuccal canal became visible, even without magnification. The orifice was extremely narrow and initially resisted the entry of even a size 6 K-file. With the use of EDTA, normal saline, and sodium hypochlorite, the file could finally glide its path to the apex. Radiographic evaluation revealed an S shaped curvature. Later, biomechanical preparation of the MB2 canal was successfully completed (Figure 3).
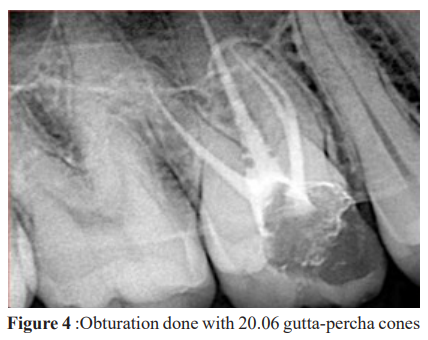
A master cone radiograph was taken, and the canals were obturated with 20.06 gutta-percha cones (Figure 4). Final radiographs were taken, and post root canal filling was completed, followed by placement of a zirconia fixed prosthesis in relation to tooth 16.
The endodontic therapy was completed in a single visit. The patient experienced mild postoperative discomfort, which resolved within 24 hours. As the patient was scheduled to travel abroad, a fixed prosthesis was delivered one week later. Follow-up evaluations at 1 month and 2 months, conducted telephonically, revealed that the patient was completely comfortable in chewing and satisfied with the aesthics.
Discussion
The maxillary first molar typically has three roots and three root canals: mesiobuccal, distobuccal, and palatal.1 However, the incidence of a second mesiobuccal canal (MB2) has been reported to range from 18.6% to 96.1%.2 In Asian population, the prevalence of MB2 canal in maxillary first molars has been reported at 58.4%.3,4
Anatomical variations in root canal systems often require the use of magnification for accurate identification. However, by carefully following and understanding the dentinal map, additional canals can sometimes be located even without magnification. Several studies have compared the effectiveness of locating canal orifices with and without the aid of magnification.5-7
Cone-beam computed tomography (CBCT) is also an important aid in studying the anatomy of a root canal.8-11 Stropko observed that the detection rate of MB2 canals in maxillary first molars can reach up to 93% when adequate clinical time, magnification, appropriate instrumentation, and thorough knowledge of their location are applied.12
Conclusion
This case confirms the need for applying fundamental rules and meticulous irrigation protocols while performing endodontic therapy. The use of advanced aids is definitely advantageous, but the clinician’s expertise in observing and interpreting what the root canal presents is of utmost importance. The success of root canal therapy lies in these details and in treating them effectively.
Conflict of interest
The authors declare no conflicts of interests.
Supporting File
References
- Gopikrishna V. Grossman's Endodontic Practice. 14th edition. Wolters Kluwer India; 2020.
- Zhang ZH, Yao HL, Zhang Y, et al. Endodontic management of the maxillary first molar with special root canals: A case report and review of the literature. World J Clin Cases 2020;8(12):2590-2596.
- Kulild JC, Peters DD. Incidence and configuration of canal systems in the mesiobuccal root of maxillary first and second molars. J Endod 1990;16:311-317.
- Vitalis A, Lip GY, Kay M, et al. Ethnic differences in the prevalence of peripheral arterial disease: a systematic review and meta-analysis. Expert Rev Cardiovasc Ther 2017;15:327-338.
- Buhrley LJ, Barrows MJ, BeGole EA, et al. Effect of magnification on locating the MB2 canal in maxillary molars. J Endod 2002;28(4):324-7.
- Coutinho Filho T, Cerda RS, Gurgel Filho ED, et al. The influence of the surgical operating microscope in locating the mesiolingual canal orifice: A laboratory analysis. Braz Oral Res 2006;20:59-63.
- Baldassari-Cruz LA, Lilly JP, Rivera EM. The influence of dental operating microscope in locating the mesiolingual canal orifice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93(2):190-4.
- Tachibana H, Matsumoto K. Applicability of x-ray computerized tomography in endodontics. Endod Dent Traumatol 1990;6:16-20.
- Kottoor J, Velmurugan N, Sudha R, et al. Maxillary first molar with seven root canals diagnosed with cone-beam computed tomography scanning: a case report. J Endod 2010;36(5):915-21.
- Abella F, Mercadé M, Duran‐Sindreu F, et al. Managing severe curvature of radix entomolaris: three-dimensional analysis with cone beam computed tomography. Int Endod J 2011;44(9):876-85.
- Kottoor J, Velmurugan N, Ballal S, et al. Four-rooted maxillary first molar having C-shaped palatal root canal morphology evaluated using cone-beam computerized tomography: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111(5):e41-5.
- Cleghorn BM, Christie WH, Dong CC. Root and root canal morphology of the human permanent maxillary first molar: A literature review. J Endod 2006;32:813-21.