RGUHS Nat. J. Pub. Heal. Sci Vol No: 17 Issue No: 4 pISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Umapathy Thimmegowda, Professor, Department of Pediatric and Preventive Dentistry, Rajarajeswari Dental College and Hospital, Ramohalli Cross, Kumbalgodu, Mysore Road, Bangalore, Karnataka, India.
2Department of Pediatric and Preventive Dentistry, Rajarajeswari Dental College and Hospital, Bangalore, Karnataka, India
3Department of Pediatric and Preventive Dentistry, Rajarajeswari Dental College and Hospital, Bangalore, Karnataka, India
4Department of Pediatric and Preventive Dentistry, Rajarajeswari Dental College and Hospital, Bangalore, Karnataka, India
*Corresponding Author:
Dr. Umapathy Thimmegowda, Professor, Department of Pediatric and Preventive Dentistry, Rajarajeswari Dental College and Hospital, Ramohalli Cross, Kumbalgodu, Mysore Road, Bangalore, Karnataka, India., Email: umapathygowda@gmail.com
Abstract
In literary works, radicular cysts have been referred to by various terms, including periapical, root end, apical periodontal, and dental cysts. They typically develop as an inflammatory response to pulp necrosis or microtrauma, originating from the epithelial cell rests of Malassez within the periodontal ligament. These lesions are usually asymptomatic and are often detected incidentally on radiographic examination. The present article reports the case of a 14-year-old female with an apical periodontal cyst associated with permanent mandibular posterior teeth. An interdisciplinary, conservative treatment approach was undertaken, preserving important structures and avoiding postoperative complications. Satisfactory healing was observed on follow-up. This case highlights the pivotal role of the pediatric dentist in the early diagnosis and interdisciplinary management of apical periodontal cysts in children.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Odontogenic cysts and tumours are significant entities in oral and maxillofacial pathology and are frequently encountered in dental practice. They can be developmental or inflammatory in origin, with radicular cysts being the most common type, usually arising as a sequela of dental caries.1
Radicular cysts, also called periapical cysts, apical periodontal cysts, root-end cysts, or dental cysts, are caused due to inflammation resulting from trauma or pulp necrosis in the periodontal ligament, affecting the epithelial cell remains of Malassez.2 The reported prevalence of radicular cysts in the primary dentition ranges from 0.5-3.3%, while in the permanent dentition, it ranges from 7-54%. They are more common in the maxilla, typically measuring 5-15 mm in diameter.3
Radicular cysts develop as a result of pulp necrosis, followed by microbial invasion and proliferation along the root canal system. The release of microbial toxins and inflammatory agents into the periapical area, together with intricate connections between epithelial and stromal cells, further contribute to cyst formation.4 Epithelial cell rests proliferate in response to this periradicular inflammation.5
A definitive diagnosis of a true cyst can only be established through histologic examination and cannot be made solely based on clinical examination or treatment outcomes. Follow-up is required after optimal root canal treatment, prior to surgical intervention. Factors like lesion size, tooth location, neighbouring anatomic structures, and the subject's overall health condition can influence periapical surgery decision-making.6 The management of radicular cysts, if clinical and radiographic signs suggest a periapical inflammatory lesion, can involve total enucleation for small lesions, marsupialization for larger cysts, or a combination of both.7
The role of the pediatric dentist in early diagnosis in crucial in reducing the risk of complications such as damage to adjacent teeth and bone. This article presents a case of an apical periodontal cyst, emphasizing the importance of early detection and multidisciplinary management by the pediatric dentist.
Case Presentation
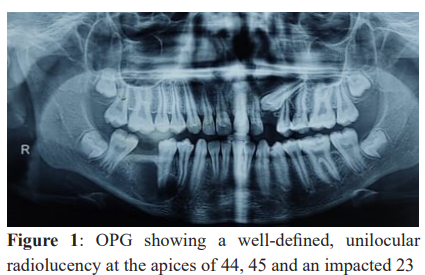
A 14-year-old female patient visited the Department of Pediatric and Preventive Dentistry with a chief complaint of pain in the lower left back tooth region for the past three days. The pain was described as sudden in onset, pricking, and continuous in nature, aggravated on chewing, and relieved only with medication. A history of night pain since three days was also reported. The patient had initially visited a private dental clinic, where an orthopantomogram (OPG) was advised. The OPG revealed a missing 46 associated with a large lesion in the lower right posterior region, as well as an impacted maxillary right canine (Figure 1). The patient was then referred to Rajarajeswari Dental College and Hospital for further evaluation. The dental history revealed trauma and tooth extraction irt 46 done at a private clinic six months back.
On intraoral examination, tooth 46 was missing, and carious lesions were noted in relation to 36, 37, and 47. No significant extraoral swelling was noted. The edentulous region of 46 was tender on palpation. Electric pulp testing and heat test were performed to determine the vitality irt 43, 44, 45 and 47. Teeth 43 and 47 elicited an immediate response, confirming vitality, while 44 and 45 showed delayed responses, suggestive of non-vital pulp. Radiographic examination with an OPG revealed a large, unilocular, well-defined, solitary radiolucency with a corticated border, extending around the apices of 44, 45 and 47. The lesion was oval in shape. Based on the clinical and radiographic findings, a provisional diagnosis of an apical periodontal cyst was made.
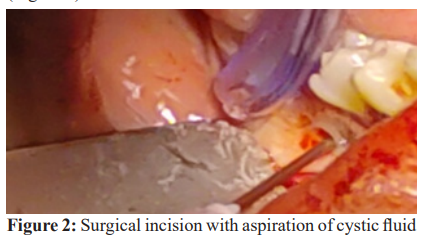
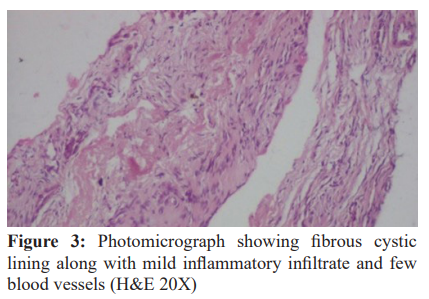
A conservative treatment approach was planned, which included aspiration of cystic fluid for histopathological investigation and endodontic management of 44 and 45 with mineral trioxide aggregate considering the open apices. Prior to treatment, routine haematological investigations were performed and the results were within normal limits. On the day of surgery, informed consent was obtained from the patient’s parent. Under local anaesthesia, cystic enucleation and curettage was performed, followed by primary closure (Figure 2). The enucleated cystic lining and aspirated fluid were collected and sent for the histopathological examination. Histopathological analysis revealed fibrous cystic wall lined by epithelium of varying thickness, with areas of hyperplastic epithelium. The presence of eosinophilic hyalinised substance resembling hyaline bodies, and mucous cells was noted. The underlying connective tissue appeared oedematous, with dense chronic inflammatory cell infiltrate and a few blood vessels, confirming the diagnosis of an apical periodontal cyst (Figure 3).
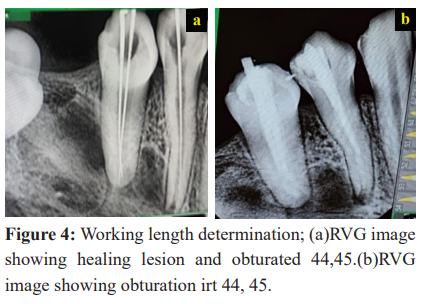
After one week, suture removal was carried out. On the same day, under local anaesthesia, access opening was performed in teeth 44 and 45, followed by canal debridement and determination of working length. A closed dressing with intracanal medicament was placed. After three weeks, radiovisiography (RVG) revealed early signs of healing of the periapical lesion, and MTA was placed as an apical barrier. At the three-month follow-up, radiographic evaluation showed a marked reduction in the size of the lesion with evidence of new bone formation. Biomechanical preparation was subsequently completed, and obturation was carried out for teeth 44 and 45 (Figure 4). The patient remains under periodic observation for further follow-up.
Discussion
The Greek word “kystis,” meaning "sac” or “bladder,“ is the origin for the word “cyst”. A cyst is characterized as a diseased hollow with an expanding, centrifugal growth mechanism, and is typically lined by epithelium.2
Radicular cysts account for approximately 52% to 68% of all jaw cysts, making them the most common cystic lesions of the jaw. They are most frequently associated with trauma or dental caries. In the present case, the patient reported a history of trauma, which may represent the probable etiological factor, although the involved teeth were not initially compromised. A plausible explanation for the disease's onset is that pulpal necrosis in a non-vital tooth triggers inflammation, which in turn activates the epithelial remnants.8 The natural course of a radicular cyst begins with a non-vital tooth that persists long enough to develop chronic periapical pathology. These lesions are most frequently discovered at the apices of the affected teeth. They are usually asymptomatic and are often detected incidentally during routine radiologic examinations.
The lesion was diagnosed as an infected radicular cyst, characterized histologically by a stratified squamous epithelium lining and a mixed inflammatory cell infiltrate. Typical features of radicular cysts include cortical expansion, root resorption, and displacement of adjacent teeth. However, in the present case, no cortical plate expansion was observed, and the adjacent teeth were non-vital.
The management of radicular cysts may involve non-surgical root canal therapy for smaller lesions or surgical approaches such as enucleation, marsupialization, or decompression for larger lesions. In the present case, a conservative multidisciplinary approach was adopted.6 Conventional root canal therapy remains the primary treatment modality for managing periapical lesions, including cysts, which can be effectively treated with non-surgical approach using intra-canal medicaments such as calcium hydroxide.9 The conservative approach involves removal of infected tissues from the cystic cavity and endodontic treatment of adjacent teeth. In this case, the procedure was carried out under local anaesthesia, followed by placement of sutures. Access openings were prepared in the involved teeth, after which biomechanical preparation and obturation following mineral trioxide aggregate (MTA) placement were undertaken. MTA has emerged as a promising alternative to calcium hydroxide, offering advantages such as reduced treatment time, immediate tooth restoration, with no adverse effects on root dentin mechanical properties. A prospective study has demonstrated high healing rates and reliable apical closure in apexification procedures using MTA.10 The study highlighted its potential as a cost-effective, easily accessible, and adjustable apical matrix for uneven healing of lesion. Regular follow-ups and radiographic evaluations are essential, as progressive reduction in lesion size confirms successful management. Early diagnosis remains crucial for the conservative management of such lesions, as it minimizes post-operative pain and enhances prognosis. Moreover, pediatric dentists play a crucial role in the early detection and interdisciplinary management of these lesions.
Conclusion
Recognition of the consequences of untreated or undiagnosed radicular cysts and their early diagnosis is crucial for preventing adverse outcomes. An interdisciplinary approach is essential to ensure effective management and favourable prognosis.
Conflict of Interest
Nil
Supporting File
References
- Neville B, Damm D, Allen C, et al. Oral and maxillofacial pathology. 3rd ed. Elsevier; 2008.
- Shear M. Cyst of the oral region. 2nd ed. Butterworth-Heinemann Ltd; John Wright and Sons; 1983.
- Schvartzman Cohen R, Goldberger T, Merzlak I, et al. The development of large radicular cysts in endodontically versus non-endodontically treated maxillary teeth. Medicina (Kaunas) 2021;57(9):991.
- Goswami M, Chauhan N. Radicular cyst with primary mandibular molar: A rare occurrence. Int J Clin Pediatr Dent 2023;16(5):769-773.
- Deshpande A Jr, Reche A, Deshpande M, et al. Radicular cyst presenting in a female child: A case report. Cureus 2023;15(9):e45872.
- Tian FC, Bergeron BE, Kalathingal S, et al. Management of large radicular lesions using decompression: A case series and review of the literature. J Endod 2019;45(5):651-659.
- Nagarathna C, Jaya AR, Jaiganesh I. Radicular cyst followed by incomplete pulp therapy in primary molar case report. J Indian Soc Pedod Prev Dent 2019;31:191-193.
- Kadam NS, Ataide Ide N, Raghava P, et al. Management of large radicular cyst by conservative surgical approach: A case report. J Clin Diagn Res 2014;8(2):239-41.
- Agrawal P, Nikhade P, Patel A, et al. Management of discoloured anterior teeth with radicular cyst: A case report. Cureus 2023;15(9):e45536.
- Purra AR, Ahangar FA, Chadgal S, et al. Mineral trioxide aggregate apexification: A novel approach. J Conserv Dent 2016;19(4):377-80.