RGUHS Nat. J. Pub. Heal. Sci Vol No: 17 Issue No: 3 pISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Sameer A Sait, Department of Conservative Dentistry and Endodontics, Maratha Mandal’s NGH Institute of Dental Sciences and Research Centre, Belagavi, Karnataka, India.
2Department of Conservative Dentistry and Endodontics, Maratha Mandal’s NGH Institute of Dental Sciences and Research Centre, Belagavi, Karnataka, India
3Department of Conservative Dentistry and Endodontics, Maratha Mandal’s NGH Institute of Dental Sciences and Research Centre, Belagavi, Karnataka, India
4Department of Conservative Dentistry and Endodontics, Maratha Mandal’s NGH Institute of Dental Sciences and Research Centre, Belagavi, Karnataka, India
*Corresponding Author:
Dr. Sameer A Sait, Department of Conservative Dentistry and Endodontics, Maratha Mandal’s NGH Institute of Dental Sciences and Research Centre, Belagavi, Karnataka, India., Email: dr.sameersait@gmail.com
Abstract
Long-standing periradicular infections can activate osteoclastic cells, leading to external inflammatory root resorption (EIRR). Delayed intervention may result in excessive loss of root structure, compromising the long-term prognosis of the affected tooth. This case report describes the successful management of EIRR associated with periradicular radiolucency in a maxillary first molar using mineral trioxide aggregate (MTA) as an apical barrier, followed by completion of root canal treatment. Preoperative radiographic and cone-beam computed tomographic (CBCT) evaluations facilitated accurate diagnosis and guided an appropriate treatment plan. At the one-year follow-up, the patient remained asymptomatic, and radiographic examination demonstrated significant bone healing.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Bacteria and their endotoxins present in an infected root canal system can reach the periradicular tissues through the apical foramen or lateral canals. The microbial agents elicit an inflammatory reaction which, if left untreated, can progress to a chronic infection. Persistent inflammatory response may activate clastic cells, leading to resorption of the tooth structure and adjacent bone, a condition known as external inflammatory root resorption (EIRR).1
A thorough understanding of the pathophysiology of the resorptive process is essential for accurate diagnosis and effective management of such cases. Radiographic evaluation, including the cone-beam computed tomography (CBCT), can be invaluable in the diagnosis of such conditions.
This article presents the management of a maxillary molar exhibiting EIRR of the palatal root, treated through non-surgical root canal treatment and mineral trioxide aggregate (MTA) apexification.
Case Presentation
A 25-year-old male patient reported to the Department of Conservative Dentistry and Endodontics, with a chief complaint of decay and pain in the right upper back tooth region. The patient's medical history was non-contributory. Clinical examination revealed deep occlusal caries in tooth #16. Radiographic evaluation showed a radiolucent area involving the pulp space and periradicular region (Figure 1A). Pulp sensibility tests using cold and heat stimuli elicited no response from the offending tooth. Based on these findings, root canal treatment followed by full-coverage crown restoration was planned for tooth #16.
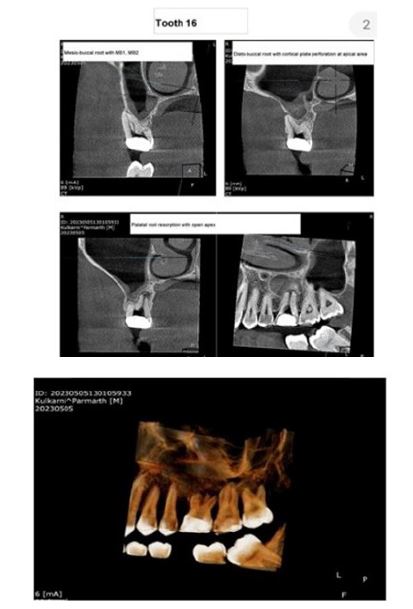
Informed consent was acquired from the patient, following which root canal treatment was initiated for tooth #16 under local anesthesia using 2% lidocaine with 1:80,000 epinephrine (La-Force, Vishal, India). Access was gained using an Endo access bur (Dentsply Maillefer, Ballaigues, Switzerland) mounted on a high-speed handpiece, and the cavity was refined with an Endo-Z bur (Dentsply Maillefer, Ballaigues, Switzerland). Four canal orifices-mesiobuccal 1, mesiobuccal 2, distobuccal, and palatal-were located (Figure 1B). The palatal root showed signs of a wide open apex, prompting referral for a CBCT scan. The CBCT revealed a chronic periapical abscess and external root resorption associated with the palatal root of tooth #16 (Figure 2). Consequently, an apexification procedure was planned for the palatal root, followed by obturation and placement of a full-coverage crown.
Root canal treatment was continued for tooth #16. Working length determination was done using K-files (Mani Inc., Tochigi-Ken, Japan) and an electronic apex locator (Eighteeth E-pex, Changzhou, China), and later confirmed radiographically (RVG). Radiographic working length verification was done using Ingle’s method, and Weine’s modification was applied for the palatal canal, wherein 2 mm was subtracted from the radiographic apex (Figure 1C).2,3 Biomechanical preparation was performed using nickel-titanium rotary files. The mesiobuccal-1 and mesiobuccal-2 canals were instrumented up to ProTaper Gold F1, and the distobuccal canal was enlarged up to Protaper Gold F2 (Dentsply Maillefer, Ballaigues, Switzerland), with intermittent irrigation using 3% sodium hypochlorite (Prime Dental Products Pvt. Ltd., Thane, Maharashtra) and normal saline. The palatal canal was instrumented with a No. 70 K-file (Mani Inc., Tochigi-Ken, Japan) (Figure 1D) and irrigated with 2% chlorhexidine gluconate (Waldent, India) followed by normal saline. A calcium hydroxide intracanal medicament (RC Cal, Prime Dental Products Pvt. Ltd., Thane, Maharashtra) was placed and the access cavity was sealed with Cavit (3M ESPE, Seefeld, Germany). The dressing was maintained for two weeks, with replacement at one-week intervals.
After two weeks, the patient was asymptomatic, and radiographic evaluation revealed a reduction in the size of the periapical lesion. Apexification of the palatal root was performed using MTA (ProRoot MTA White, Dentsply Sirona, Ballaigues, Switzerland) (Figure 1E). The MTA was condensed using a hand plugger RCP60 (GDC, India) and micro-applicator tips moistened with normal saline. Radiographs were taken intermittently to verify proper apical positioning of MTA. A moist cotton pellet was placed over the MTA, and the access cavity was sealed temporarily with Cavit (3M ESPE, Seefeld, Germany). The patient was recalled after two days, at which time an apical stop (seal) was confirmed using a No. 70 K-file (Figure 1F). The MB-1, MB-2, and DB canals were re-instrumented to the last used files and irrigated with 3% sodium hypochlorite (Prime Dental Products Pvt. Ltd., Thane, Maharashtra) followed by normal saline. The palatal canal was re-instrumented using a No. 70 K-file and irrigated with 2% chlorhexidine gluconate (Waldent, India) and normal saline. All canals were then dried with sterile paper points (Meta Biomed, Cheongju, South Korea). Obturation of the MB-1, MB-2, and DB canals was performed using the single cone gutta-percha points (Meta Biomed, Cheongju, South Korea) and AH plus sealer (Dentsply Maillefer, Ballaigues, Switzerland) (Figure 1G). The palatal canal was obturated using the cold lateral condensation technique. Post-endodontic restoration was completed with Miracle Mix (GC Fuji, Japan) (Figure 1G).
At the one-month follow-up, the patient remained completely asymptomatic. Radiographic evaluation revealed satisfactory bone healing, evidenced by a marked reduction in the periapical radiolucency. A full-coverage porcelain-fused-to-metal (PFM) crown was planned and subsequently placed on tooth #16 during this period (Figure 1H).
Discussion
EIRR is the most prevalent form of external root resorption and typically remains asymptomatic.4,5 The resorptive process is initiated by an inflammatory response caused by the bacteria and/or their endotoxins reaching the periradicular space. Although EIRR most commonly affects the apical region of the tooth, it can occur at any level along the length of the root due to the presence of accessory or lateral canals, which can serve as alternate pathways for bacterial dissemination.1,6 MTA was introduced in 1993 by Torabinejad et al. as a root-end filling material, owing to its superior sealing ability as compared with the then widely used amalgam. It also overcame the inherent drawbacks of amalgam, such as initial leakage, secondary corrosion, mercury and tin contamination, need for mechanical retention in the root-end preparations, staining of hard and soft tissues.7 Unlike amalgam, MTA does not require maintenance of a dry field; in fact, the requirement of moisture for its hardening further contributes to its success as a root-end filling material. Since its introduction, MTA has been widely used with success in procedures like pulp capping, apexification, root-end filling (both orthograde and retrograde), and the repair of perforations.7-9
In the present case, resorption of the palatal root and the presence of a wide open apex limited the use of nickel-titanium rotary files; therefore, No. 70 K-file was used for the biomechanical preparation. Also, due to the potential cytotoxic effects of sodium hypochlorite when extruded beyond the apex, it was not used for irrigation of the palatal canal. Instead, 2% chlorhexidine gluconate was employed as an irrigant due to its superior biocompatibility compared with sodium hypochlorite.10,11
At the one-month follow-up, the patient remained asymptomatic, and radiographic evaluation demonstrated satisfactory bone healing. Consequently, a full-coverage PFM crown was placed on the treated tooth. The rapid periradicular healing observed can be attributed to the osteoinductive potential of MTA when used as an apical filling material.12
At the six-month and one-year follow-up appointments, the patient continued to be asymptomatic, and radiographic evaluation revealed almost complete reduction of the periradicular radiolucency (Figure 1).
External inflammatory root resorption, if left untreated, can lead to significant loss of tooth structure and compromise the long-term prognosis. Accurate diagnosis, followed by conventional non-surgical root canal therapy utilizing an appropriate irrigation protocol, intermediate calcium hydroxide dressings, and MTA as an apical barrier material, can effectively arrest the resorptive process and promote periradicular healing, thus providing an overall successful clinical outcome in the management of EIRR cases.
Conflict of interest
None
Source of funding
Nil
Supporting File
References
1. Sait S, Uppin V, Pujar M, et al. Revisiting external tooth resorption. Paripex - Indian Journal of Research 2023;12(8):65-69.
2. Weine FS. Endodontic therapy. 5th Ed. St. Louis: Mosby; 1996. p. 398.
3. Ingle JI, Bakland LK. Endodontic cavity preparation. In: Textbook of endodontics. 5th ed. Philadelphia: BC Decker; 2002.
4. Abhilash R, Balan J, Shoba K, et al. External inflammatory root resorption: Management of a tooth with hopeless prognosis. Cons Dent Endod J 2017;2(1):24-27.
5. Nayak MT, Nayak A. External inflammatory root resorption in mandibular first molar: A case report. Malays J Med Sci 2015;22(6):63-66.
6. Abbott PV, Lin S. Tooth resorption-Part 2: A clinical classification. Dent Traumatol 2022;38:267-285.
7. Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod 1993;19(12): 591-5.
8. Purra AR, Ahangar FA, Chadgal S, et al. Mineral trioxide aggregate apexification: A novel approach. J Conserv Dent 2016;19(4):377-80.
9. Cervino G, Laino L, D'Amico C, et al. Mineral trioxide aggregate applications in endodontics: A review. Eur J Dent 2020;14(4):683-691.
10. Perotti S, Bin P, Cecchi R. Hypochlorite accident during endodontic therapy with nerve damage - A case report. Acta Biomed 2018;89(1):104-108.
11. Gomes BP, Vianna ME, Zaia AA, et al. Chlorhexidine in endodontics. Braz Dent J 2013;24(2): 89-102.
12. Gandolfi MG, Iezzi G, Piattelli A, et al. Osteo-inductive potential and bone-bonding ability of ProRoot MTA, MTA Plus and Biodentine in rabbit intramedullary model: Microchemical characterization and histological analysis. Dent Mater 2017;33(5):e221-e238.