RGUHS Nat. J. Pub. Heal. Sci Vol No: 17 Issue No: 2 pISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
Dr. Shilpa.S.Sasalawad1 , Dr. Srinath.S.K2 , Dr. Sahana3 , Dr. Nihal R Kothari4
1: Assistant professor, Dept of Paediatric and Preventive dentistry, Government Dental College and Research Institute, Bengaluru 560002 2: Professor and Head, Dept of Paediatric and Preventive dentistry, Government Dental College and Research Institute, Bengaluru 560002 3: Professor and Head, Dept of Oral Pathology and Microbiology, Government Dental College and Research Institute, Bengaluru 560002 4: Post Graduate student, Dept of Paediatric and Preventive dentistry, Government Dental College and Research Institute, Bengaluru 560002
Address for correspondence:
Dr. Nihal R Kothari
Post Graduate student Dept of Paediatric and Preventive dentistry Government Dental College and Research Institute Bengaluru 560002 Email id: nihalkothari44@gmail.com Phone number: 8123693115

Abstract
Fibrous dysplasia (FD) is a fibro-osseous anomaly, where in normal bone is substituted with fibrous stroma. It is of unknown etiology but recently reported to be associated with mutation in GNAS1 gene (20q13.2) and consists of three subtypes monostotic, polyostotic and craniofacial. Craniofacial FD (CFD) mainly affects the bones of the craniofacial skeletal frame. This article reports a case of a 10 year old boy diagnosed with polyostotic fibrous dysplasia with clinical, radiographical and tissue pathological features.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Fibrous dysplasia (FD) is a fibro-osseous anomaly, where in normal bone is substituted with fibrous stroma.1 It is a developmental disorder of the bone due to defect in osteoblastic differentiation and maturation, and can affect any bone in the body. It is a nonhereditary disorder of unknown cause, but now it has been thought to be associated with mutation in the GNAS1 gene (20q13.2).2 Fibrous dysplasia starts in childhood, presenting with a slowly progressive enlargement of bone that generally slows or ceases with puberty.1 Several forms of fibrous dysplasia have been described, Monostotic form, Polyostotic form and Craniofacial form. Craniofacial form affects the bones of the craniofacial complex, including the upper and lower jaw. The diagnosis of FD is depends on clinical, radiological, and histopathological examination. Different treatment approaches include observation, medical treatment, and surgical treatment.
Case report
A 10 year old boy reported to the department of pediatric dentistry with chief complaint of painless swelling in the middle third of the face on right side, since childhood which increased abruptly over a month. Medical and family histories were not relevant. There was negative history of trauma to face. Extra oral examination revealed obvious facial dissymmetry with bony hard swelling on the right zygomatic and maxillary region with no extra oral discharge or sinus opening (Figure 1a & 1b). Skin over swelling appeared normal. Swelling was bony hard and tender on palpation. Intra orally, no carious teeth were present. Spacing between the teeth in the right maxilla region was noted. Enlargement of buccal cortical plate on right side of maxilla, with obliteration of right buccal vestibule was seen (Figure 2). Serial axial CT sections of facial bones was performed, ill defined bone expansion was seen in the right maxillary sinus effacing the sinus space. Lesion in maxillary sinus measured 32x34x34 mm, involving anterior 1/3rd of right zygomatic arch, pterygoid plates, floor of middle cranial fossa, bony walls of sphenoid sinus, right posterior ethmoid air cells, perpendicular plates of ethmoid and cristae galli (Figure 3). Similar expansion in medullary region of size 62x13x12 mm was seen in right body of mandible, with ground glass appearance. No break in cortical plate was noted. A provisional diagnosis of fibrous dysplasia was made and Paget’s disease as differential diagnosis.Biochemical findings showed raised levels of serum Alkaline Phosphatase enzyme.
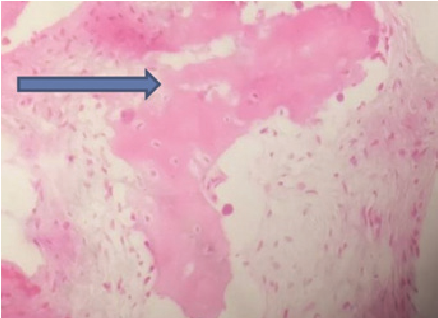
A piece of tissue from the buccal vestibule in maxillary region was excised for tissue pathology, microscopic examination shows cellular fibrous connective tissue stroma intermixed with irregular immature bony trabeculae. The bone is in curvilinear pattern and osteoblastic rimming is absent. Areas of reversal and resting lines have been noticed (Figure 4).
Histopathological and radiographical findings suggested fibrous dysplasia. A confirmatory diagnosis of polyostotic fibrous dysplasia was established on clinical, radiograph, histopathological findings. Cosmetic correction will be done if required after puberty, as most of the cases undergo regression after puberty.
Discussion
Fibrous dysplasia (FD) is a rare nonhereditary skeletal anomaly characterized by excessive proliferation of cellular fibrous connective tissue intermixed with irregular bony trabeculae.3 A mutation in the GNAS1 gene (20q13.2) is found to be associated with the tumor. The GNAS1 (guanine nucleotidebinding protein, -stimulating activity polypeptide) gene encodes a G-protein that stimulates the production of cAMP. The mutation results in a continuous activation of the G-protein leading to overproduction of cAMP in affected tissues. This results in a hyperfunction of affected endocrine organs, frequently giving rise to precocious puberty, hyperthyroidism, growth hormone and cortisol overproduction. There is an increased proliferation of melanocytes that cause large café-au-lait spots with irregular margins. cAMP affects the differentation of osteoblasts leading to fibrous dysplasia. In fibrous dysplasia, abnormal fibrous tissue replaces the medullary bone, which gives a characteristic radiographic appearance described as ground-glass appearance.2 FD commonly affects children and young adults. Approximately 20–30% of fibrous dysplasias are polyostotic. Craniofacial skeletal bones are affected in approxiamately 30% of cases. Often, the initial symptom is pain in the involved bone, spontaneous fracture, or both. There may be expansion and deformity of the jaws, and the eruption pattern of the teeth is disturbed because of the loss of normal support of the developing teeth. The endocrine disturbance also may alter the time of eruption of the teeth.2 There are no standard treatment protocols known to exist for FD. The primary aim is to correct function and aesthetics of the patient. Surgical excision of the affected bone tissue is usually a successful way of treatment, however drawback is, a large aesthetic and functional paucity, with long-term postoperative effects.4 In stable lesions, the patient is kept under observation until puberty.3 The conservative management with confined reduction in the size of these lesions is sufficient to alleviate the symptoms.4
In present case, patient had no endocrine disturbances and café-au-lait spots were not present. After a confirmatory biopsy, our case was diagnosed with polyostotic fibrous dysplasia. The treatment of choice was conservative management with regular recall and clinical observation. The prevalence of malignant transformation of FD is reported to be 0.4%–4%. Therefore, periodic follow‑up, for every 6 months and radiographic investigation should be carried out to verify that there is no progression or malignancy transformation.5 Cosmetic correction if required will be carried out after completion of puberty.
Conclusion
Craniofacial polyostotic fibrous dysplasia is rare, with varied clinical and radiographic appearances. Definite diagnosis can be achieved by radiographical and histopathological reports. Management of the lesion is mainly conservative since the tumor regresses with age. Rate of recurrence and malignant transformation is high, thus long term follow- up is mandatory in these cases.
Figure Legends
Figure 1: 1a: Front view of the patient illustrating swelling on the right middle third of face.
1b: lateral view showing enlargement on the right side of maxillary region.
Figure 2: Spacing between the teeth and expansion of buccal cortical plate.
Figure 3: CT sections of facial bones showing ill defined bone expansion in medullary region with ground glass appearance in maxilla, mandible, right zygomatic arch, pterygoid plates, floor of middle cranial fossa, bony walls of sphenoid sinus, right posterior ethmoid air cells , perpendicular plates of ethmoid and cristae galli.
Figure 4: Histopathological section showing connective tissue stroma intermixed with irregular immature bony trabeculae.
Supporting File
References
- Kerr R Phelan J Burket’s Oral Medicine 11TH ED Hamilton 2008.
- Rajendran, Sivapathasundharam Shafer’s Textbook of Oral Pathology, 7th ed Elsevier 2012.
- Chandavarkar V, Patil PM, Bhargava D, Mishra MN. A rare case report of craniofacial fibrous dysplasia. J Oral Maxillofac Pathol 2018;22:406- 9.
- Cholakova RP,. Kanasirska N. Kanasirski Iv. Chenchev A. Fibrous dysplasia in the maxillomandibular Region – case report. J of IMAB 2010: 16(4).
- Yang HY, Su BC, Hwang MJ, Lee YP. Fibrous dysplasia of the anterior mandible: A rare case report. Tzu Chi Med J 2018;30:185-7